Atrial fibrillation
What is Atrial Fibrillation (AFib or AF)?
Atrial fibrillation (AF) is a rapid and irregular heart rhythm (arrhythmia) caused by faulty electrical signals from the upper chambers of the heart (atria). Electrical signals should normally originate only from the sinus node (the heart’s natural pacemaker), creating a steady heart rhythm – about 60 to 100 beats per minute. AF is marked by rapid electrical signals that come from the atria, causing them to quiver instead of contract properly. These electrical signals may increase the heart rate to 100 to 175 beats per minute or more.
AF is the most common type of sustained arrhythmia, affecting 2 million people each year in the United States alone. The American Heart Association (AHA) notes that hospitalizations for AF have tripled since 1985. The risk of developing atrial fibrillation increases dramatically with age. As a result, approximately 70 percent of patients with atrial fibrillation are between the ages of 65 and 85 years old.
Not all abnormal heartbeats are a sign of AF. Skips, pauses or unusually strong/irregular heartbeats (palpitations) commonly occur in people with no history of heart problems.
Some are related to more serious cardiac problems, while others are not.
A rhythm that is closely related to atrial fibrillation is atrial flutter, in which a very rapid but regular electrical signal in the atria causes a very rapid heartbeat.
It is common for patients to experience episodes of atrial fibrillation at some times and atrial flutter at others. Like atrial fibrillation, atrial flutter increases the risk of stroke. According to the AHA, it leads to more than 54,000 deaths in the United States each year. People who experience abnormal or irregular heartbeats are encouraged to speak with their physician.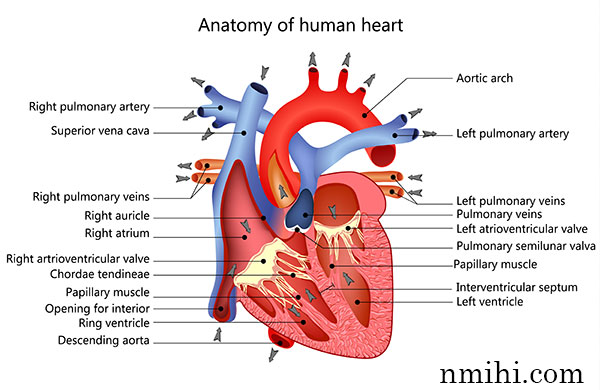 There are several dangerous conditions associated with atrial fibrillation. Among the most common is the risk of blood clots forming in the atria as they quiver. If part of a clot breaks off and leaves the heart via the arteries, it can become lodged in blood vessels that supply the brain, lungs or other parts of the body with blood. Depending upon where the traveling blood clot (embolus) becomes lodged, the patient could experience symptoms ranging from cold feet to a stroke. Atrial fibrillation is also associated with heart failure.
There are several dangerous conditions associated with atrial fibrillation. Among the most common is the risk of blood clots forming in the atria as they quiver. If part of a clot breaks off and leaves the heart via the arteries, it can become lodged in blood vessels that supply the brain, lungs or other parts of the body with blood. Depending upon where the traveling blood clot (embolus) becomes lodged, the patient could experience symptoms ranging from cold feet to a stroke. Atrial fibrillation is also associated with heart failure.
The risk associated with atrial fibrillation depends on the duration of the condition. The American College of Cardiology, along with the AHA, has proposed the following classification system for atrial fibrillation:
- Paroxysmal atrial fibrillation, in which the arrhythmia lasts less than seven days and usually less than 24 hours and may be recurrent.
- Persistent atrial fibrillation, in which the arrhythmia lasts longer than seven days, but the abnormal rhythm can be stopped with treatment (e.g., cardioversion with a defibrillator).
- Permanent atrial fibrillation, in which the arrhythmia lasts longer than one year and has either not responded to treatment or treatment has not been attempted.
- Lone atrial fibrillation, in which the arrhythmia, either paroxysmal or persistent, occurs in people without any other form of heart disease.
A quite different (and life-threatening) condition is ventricular fibrillation (VF). Ventricular fibrillation involves a quivering of the ventricles instead of the atria. Unlike atrial fibrillation, ventricular fibrillation is life threatening because it results in a heart rate of 350 beats per minute or higher. Because of these rapid, chaotic contractions, the heart is unable to pump blood to the body. Untreated, ventricular fibrillation can result in sudden cardiac death within minutes. Treatment for ventricular fibrillation involves shocking the heart back into a normal rhythm with a defibrillator. Among high-risk patients, implantable cardioverter defibrillators continuously monitor the heart and deliver a shock when necessary.
Some patients have a condition that allows extra impulses to travel between the atrium and ventricles (this is known as Wolf Parkinson White syndrome). In this case, atrial fibrillation is considered a risk factor for ventricular fibrillation, and episodes of atrial fibrillation can lead to a life-threatening ventricular arrhythmia.
Signs and symptoms of atrial fibrillation
Symptoms are rarely present in patients with brief episodes (e.g., less than 48 hours) of atrial fibrillation.
Among patients with episodes of longer duration, symptoms may include:
- Palpitations (heartbeats that are rapid, pounding, forceful, uncomfortable or in some way obviously irregular)
- Dizziness
- Fainting (syncope)
- Increased urination
- Low blood pressure (hypotension)
- Weakness
- Fatigue
- Shortness of breath (dyspnea)
- Chest pain that may or may not be angina
Risk factors and causes of atrial fibrillation
Atrial fibrillation (AF) is directly caused by inconsistent signals in the heart’s electrical system. Numerous conditions may cause these signals to become irregular.
Some conditions that may contribute to AF and are considered risk factors for the condition include:
- High blood pressure
- Coronary artery disease
- Previous heart attack
- Valvular heart disease
- Congenital heart defects, including valve abnormalities
- Cardiomyopathy
- Diabetes
- Other arrhythmias, including atrial flutter and ventricular fibrillation
- Inflammation. This occurs commonly after heart surgery, such as bypass surgery, and less commonly with infections such as pericarditis
- Lung problems or disease, including pulmonary embolisms
- Excessive alcohol use
- Thyroid disease
- Viral infections
- Obesity
Many other factors may potential relate to atrial fibrillation, including the use of various drugs or supplements. Recent research has indicated a connection between atrial fibrillation and the presence of Helicobactor pylori, a bacterium that causes peptic ulcers. About 5 percent of the general population harbors this bacterium in their stomachs. In a research study, more than 90 percent of patients with atrial fibrillation had the H. pylori bacteria.
Diagnosis methods for atrial fibrillation
Brief episodes of atrial fibrillation (AF) are known as paroxysmal atrial fibrillation. These episodes occur for a few minutes to a few hours before the heart returns to a normal rhythm. Paroxysmal AF is harder to diagnose because it is rarely associated with symptoms. Persistent or permanent AF, which can persist for months or years, is easier to diagnose.
There are a variety of ways to diagnose AF. For example, the physician may use a stethoscope to listen for abnormal heart rhythms. Additional tests that may be ordered include:
EKG (electrocardiogram)
An electrocardiogram (EKG) is a recording of the heart’s electrical activity as a graph on a moving strip of paper or video monitor. The pattern that is generated by the electrical impulses reveals whether the heart rhythm is normal or if the heart muscle is damaged.
Holter monitor
A continuous EKG is temporarily attached to an ambulatory (freely moving) patient for a 24-hour period (though it can be used for up to five days). This test can detect or diagnose abnormal heartbeats (arrhythmias), as well as cardiac ischemia. It can also help evaluate the effectiveness of any medications, especially antiarrhythmics, the patient may be taking.
Blood tests
These tests measure blood oxygen levels, electrolytes and other possible indicators of an underlying cause of AF.
Thyroid hormone test
Studies have shown that hyperthyroidism is commonly associated with atrial fibrillation. Patients experiencing their first suspected episode of atrial fibrillation will also likely be asked to undergo a thyroid test.
Stress test
An electrocardiogram is performed while the patient exercises in a controlled manner on a treadmill or stationary bicycle at varied speeds and elevations. The reaction of the heart under exertion can be measured and evaluated. It may be ordered to assess the extent of artery damage and/or coronary artery disease.
Echocardiogram of the heart and major arteries
This test uses sound waves to track the structure and function of the heart. A moving image of the patient’s beating heart is played on a video screen, where a physician can study the heart’s thickness, size and function. The image also shows the motion pattern and structure of the four heart valves, revealing any potential leakage (regurgitation). During this test, a Doppler ultrasound may be performed to evaluate blood flow in the heart’s chambers, the blood vessels of the arms and legs, and the carotid arteries in the neck. An echocardiogram is useful in detecting structural abnormalities that lead to atrial fibrillation. The evaluation of heart function is also helpful in selecting antiarrhythmic medicines, if needed.
Transesophageal echocardiography (TEE)
This test uses a small transducer attached to an endoscope that is inserted through the patient’s mouth and throat, and into the esophagus (the long tube from the throat to the stomach). This will not affect the patient’s ability to breathe freely but might temporarily interfere with swallowing. Once positioned, the transducer can transmit a clear image of the heart’s size and function. It may be used to detect blood clots in the atria. It also allows better assessment of the structure and function of the heart valves.
Electrophysiology study (EPS)
A test that involves an electrode catheter that is fed through a blood vessel and into the atria and ventricles. Once in place, electrical activity is recorded to assess the presence and source of abnormal heart rhythms, or to see if there has been any progress from medical treatments.
Treatment options for atrial fibrillation
As with any arrhythmia, treatment of atrial fibrillation (AF) depends on the nature and severity of the abnormal rhythm, as well as the nature of any underlying condition(s). Treating AF frequently includes treating the underlying condition, such as high blood pressure or heart failure. Not all patients with AF need to be converted to a normal rhythm.
In general, there are two approaches to treating AF.
They include:
- Rhythm control, which includes restoring the heart’s sinus rhythm.
- Rate control, which includes controlling the heart’s ventricular rate in patients with persistent or permanent atrial fibrillation.
In addition, physicians will attempt to prevent blood clots from forming and/or breaking off and traveling through the blood stream (embolizing), where they may cause stroke.
The choice of therapy depends on the patient’s condition and the nature of the atrial fibrillation. Medications that may be used include:
Beta blockers, calcium channel blockers and digoxin (a type of inotrope)
These are commonly used in rate control of atrial fibrillation. These medications slow transmission of electrical impulses from the atria to the ventricles. Though these medications slow the overall heart rate during atrial fibrillation, they will not restore the heart to its normal rhythm. Beta blockers have shown to be useful in preventing arrhythmias following heart surgery.
Antiarrhythmics
These are commonly used in rhythm control of atrial fibrillation. These medications stabilize the heart rhythm, helping to maintain a normal rhythm. There is a wide variety of antiarrhythmics that may be used, depending on the patient’s condition, mostly their heart, lung and kidney function. Antiarrhythmics can also cause undesirable side effects so patients on these medications need to see their physician regularly.
Anticoagulants
Medications that inhibit the formation of blood clots. Anticoagulants are often administered before rhythm control in initiated to prevent existing blood clots from breaking loose or new ones from forming. It is usually also continued for several weeks after therapy has begun. Anticoagulants must be monitored carefully to avoid side effects such as bleeding.
Aspirin
Aspirin acts as an antiplatelet and may be given in conjunction with anticoagulants to prevent further cardiovascular complications.
More invasive treatments include:
Cardioversion
Returns AF to a normal heart rhythm through either an electric shock or drugs. While most patients can be electrically cardioverted to a normal rhythm, only 60 percent can be maintained in a normal rhythm long term. Once again, anticoagulant therapy is frequently administered in conjunction with cardioversion. In patients who have atrial fibrillation for more than 48 hours, cardioversion should not be performed unless the presence of a clot inside the heart is excluded by a transesophageal echocardiogram and/or after three to four weeks of therapeutic treatment with warfarin (an anticoagulant).
Radiofrequency ablation
Destroying (ablating) the tissues and pathways that are causing faulty signals. Recent research has identified the pulmonary veins in the left atrium as the trigger for AF in some patients. New techniques to isolate the pulmonary veins are being developed. This technique has some risks and is reserved for patients whose symptoms persist despite medical therapy.
Pacemaker
A device that is usually implanted to keep the heart from beating too slowly. In patients with AF, a pacemaker may be used in conjunction with medication to help control the heart rate. Some types of pacemakers have special features to help suppress AF. In addition, in patients whose AF cannot be controlled with medications, the physician may perform a procedure to interrupt the electrical connection between the atrium and ventricles. This is called an AV node ablation. Afterward, the physician would implant a pacemaker to keep the heart from beating too slowly. The patient would still be in AF but not feel it.
Maze procedure
Making small, careful cuts in the atrial wall, thus designing a maze of new pathways through which electrical signals can travel. Signals will travel through this newly created maze rather than randomly leaping from various parts of the heart, therefore reducing AF. The maze procedure is highly successful. Significant research is ongoing, including the use of minimally invasive techniques and robotic procedures. The procedure is usually done in conjunction with valve surgery. The left atrial appendage, which is a structure within the left atrium that commonly harbors thrombi, is usually obliterated or excised during this surgery.
Prevention methods for atrial fibrillation
Many of the risk factors that relate to atrial fibrillation (AF) are associated with other cardiac conditions (e.g., coronary artery disease, valvular heart disease and high blood pressure). Practices that can help prevent those conditions may also help prevent AF. These include maintaining a healthy weight, eating a heart-healthy diet and exercising regularly.
Researchers are studying cases of atrial fibrillation that develop after heart surgery. Some of these cases are related to inflammation, so researchers are studying the use of anti-inflammatory drugs after surgery to decrease the likelihood of atrial fibrillation.
Atrial fibrillation may also be caused by periods of heavy drinking. Holiday heart syndrome is a condition in which individuals develop atrial fibrillation after heavy alcohol use. If the person is young and has no other underlying heart disease, including alcoholic heart disease, the heart rhythm will usually return to normal in a few hours. Treatment is usually unnecessary in these people. Those who do not have underlying coronary heart disease may be at increased risk for a heart attack once the rapid and irregular alcohol-induced rhythm develops. Most people experiencing holiday heart syndrome have no real knowledge as to whether they have underlying heart disease. Therefore, anyone experiencing this abnormal heart rhythm (arrhythmia) should seek immediate medical attention.
People are encouraged to speak with their physician if they feel a flutter, skipped beat or any other unusual beat activity. Those who continue to experience symptoms of AF even after treatment are also urged to contact their physician immediately. Many AF patients are able to live normal, active lives.
Questions for your doctor
Preparing questions in advance can help patients have more meaningful discussions with their physicians about their conditions. Patients may wish to ask their doctors the following questions related to atrial fibrillation (AF):
- I have noticed no heart changes. How can you tell I have atrial fibrillation?
- I sometimes feel some flutterings in my chest. Is that atrial fibrillation?
- Will certain conditions bring on an attack of atrial fibrillation?
- I have experienced atrial fibrillation since my bypass surgery. Will it go away on its own?
- Can you tell what type of AF I have? Is one type more dangerous than others?
- How can I tell if antiarrhythmia medicines are working? Are there side effects?
- How risky is a surgical procedure for fibrillation?
- Is cardioversion painful?
- Will treating my valve disease affect the atrial fibrillation?
- How serious does AF have to be to treat it surgically?
Additional Information
Medications
- Heart medications, such as digitalis, quinidine, calcium-channel blockers or beta-adrenergic blockers to regulate the heartbeat.
- Anticoagulants to prevent blood clot.
Activity
- Resume your normal activities as soon as symptoms improve.
- A regular exercise program is recommended.
Diet
- Lose weight if you are obese, but don't use appetite suppressants. These may worsen rhythm disturbances.
- The underlying heart condition may require a low-salt or low-fat diet and potassium supplements.
What might complicate it?
- Acute pulmonary edema.
- Arterial thrombosis or embolus.
- Congestive heart failure.
- Other heartbeat irregularities that could trigger cardiac arrest.
Alternatives
Atrial fibrillation can be a warning sign of other heart conditions such as mitral stenosis (Wolff-Parkinson-White syndrome) or thyrotoxicosis (a toxic thyroid condition). Differential diagnoses of atrial fibrillation include atrial flutter with block, shifting pacemaker associated with multifocal atrial ectopic beats, and paroxysmal atrial tachycardia. Differential diagnoses of atrial flutter include paroxysmal atrial tachycardia with variable block, ventricular tachycardia, and atrial fibrillation with block.
Notify your physician if
- You or a family member has symptoms of atrial fibrillation.
- The following occur during treatment:
- Change in heart rate, rhythm or strength.
- Chest pain, sweating and weakness.
- Shortness of breath and swollen feet and ankles.
- Pain in the calf of the leg while walking.
- New, unexplained symptoms develop. Drugs used in treatment may produce side effects.
